Endometriosis and the Gut, A Powerful Connection
Endometriosis.
You’ve likely heard this term before, but do you know what it is? Perhaps you know someone who has been afflicted by this painful disorder. Or maybe, you’re an endometriosis warrior yourself.

The prevalence of endometriosis is estimated at 10% of reproductive women worldwide.
That’s 1 in 10 females between the ages of 12 and 52, impacting roughly 196 million individuals across the planet!
The exact cause of endometriosis is still unknown, although several hypotheses exist. More over, there is currently no cure, only various treatment options we will discuss further along in this article.
Let’s take a deep dive into what endometriosis is exactly and the unique connection this disease has with the gut microbiome.
What is Endometriosis?
Endometriosis is a chronic inflammatory disease where uterine-like tissue grows outside the uterus, most often in the pelvic region, fallopian tubes, and ovaries. This abnormal growth can also occur in the intestines or any areas between the bladder, uterus, vagina, and rectum. Another term for uterine-like tissue growth is an endometrial lesion. 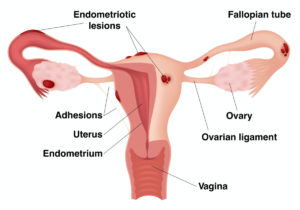 The name endometriosis originates from the anatomical term endometrium, which is the mucosal membrane lining the inside of the uterus. It’s the endometrium that thickens, breaks down, and bleeds during the menstrual cycle. A helpful tip for remembering endometrium is that ‘endo’ refers to inside, and ‘metrium’ refers to uterus.
The name endometriosis originates from the anatomical term endometrium, which is the mucosal membrane lining the inside of the uterus. It’s the endometrium that thickens, breaks down, and bleeds during the menstrual cycle. A helpful tip for remembering endometrium is that ‘endo’ refers to inside, and ‘metrium’ refers to uterus.
To explain further, when someone has endometriosis, the endometrial-like tissue growing outside the uterus acts the same way it would inside the uterus. This includes the thickening, breaking down, and bleeding. Except now, the broken-down tissue cannot exit the body and becomes trapped. Unfortunately, this can lead to cysts forming in the ovaries, scar tissue and adhesions developing in surrounding tissue, and many other complications related to inflammation and dysfunctional immune response.
Endometriosis Symptoms
The primary symptom of endometriosis is chronic pelvic pain, which becomes heightened during menstrual periods. Although many women, including those without endometriosis, experience some form of cramping during their menstrual periods, those with the disorder often have menstrual pain far more severe than average. As if the menstrual pain wasn’t enough, periods also tend to be much heavier and longer in duration. 
Unfortunately, the pain doesn’t always end with pelvic and menstrual pain. Other symptoms of endometriosis include the following: lower back and abdominal pain, painful intercourse (dyspareunia), painful bowel movements and urination, bloating, diarrhea, constipation, nausea, vomiting, fatigue, and infertility issues. Describing endometriosis patients as warriors earlier was no exaggeration!
Endometriosis and Gut Discomfort
The list of symptoms for endometriosis is undoubtedly overwhelming, but there are more complexities to the story. Within this long list, several Endometriosis symptoms overlap with the symptoms of a common gastrointestinal (GI) disorder. Can you think of a condition with symptoms involving abdominal pain, bloating, diarrhea, and constipation?
If you haven’t guessed it already, the overlapping condition is irritable bowel syndrome (IBS), a functional gut disorder that impacts the large intestine. So, on top of all the reproductive system issues, women with endometriosis are 2-3 times more likely to have IBS. Gastrointestinal symptoms affect up to 90% of endometriosis patients, with bloating, nausea, and constipation being the most common of these symptoms.
Endometriosis and the Prevalence of IBS
Studies on endometriosis and IBS have primarily occurred in isolation, but newer research shows more similarities between the two conditions. Some of the similarities include low-grade inflammation, increased leaky gut, and increased pain sensitivity within the internal organs. From an anatomy class point-of-view, the gut (small and large intestines) and the female reproductive organs are packed in right next to each other, so their impact on one another makes sense.
For example, when someone has endometrial lesions growing around their uterus and bowel area, immense pain and discomfort can arise as the GI tract has to push food along by squeezing and releasing muscles through involuntary wave-like motions called peristalsis. Issues can also occur when food is not moving. If the large intestine becomes backed up with constipation, gas can start to build up, putting pressure on the uterus and ovaries, and thus increasing the pain of endometriosis.
As one might imagine, this symptom overlap between IBS and endometriosis can lead to a diagnostic mess. However, as the scientific community continues to learn about endometriosis, gut health, and the gut microbiome, researchers are finding more and more links between all three.
Immunity, Inflammation, and the Gut Microbiome
The gut is one of the central immune system homeostasis regulators, meaning it possesses the flexibility to respond to varying stimulation from the outside environment. The gut microbiome plays a critical role in the maintenance of our health and development of disease, impacting conditions inside and outside of the GI tract. In fact, 80% of the entire immune system is contained right inside our gut!
So, what does all this ‘immune system in our gut’ talk have to do with endometriosis? Well, we know that endometriosis is associated with a dysregulated immune system and elevated inflammatory markers. Additionally, ongoing research suggests that the gut microbiome is involved in the regulation of these inflammatory factors, which could very well influence the development of endometrial lesions. Although the precise pathway is not yet clear for how certain gut bacteria affect endometriosis, newer studies show that one’s gut health may be involved with the onset and progression of the disease.
Dysbiosis
We already know from earlier that endometriosis patients suffer from IBS, but there is yet another condition they often have called dysbiosis. Dysbiosis means the ecosystem of gut flora living in the digestive track is out of balance, usually indicating a lack of healthy bacteria. When dysbiosis is present, associations with altered immune function and inflammation occur. Specifically, those with endometriosis can have less responsive natural killer cells and regulatory T cells. They can also have greater concentrations of macrophages which promote inflammation.
The connections between the gut and endometriosis seem never ending, I know! But there is one last connection to address between the gut and endometriosis that is a critical component to this seriously complex disease.
The Estrogen-Gut Dysbiosis Connection
It is well established how much the gut microbiome impacts overall health and immunity. But did you know that your gut flora also influences hormones? The hormone of focus when it comes to the endometriosis gut connection is estrogen.
Within the digestive tract, the gut microbiome helps support estrogen metabolism using a special genetic group of bacteria called the estrobolome. The estrobolome processes and modulates estrogen levels within the body, keeping the levels in a Goldilocks state for proper health and function. However, when the gut microbiome is suffering from dysbiosis, that Goldilocks state of proper estrogen levels gets completely thrown off! The science behind how this works is rather complicated but in short, dysbiosis in the gut can cause an increase of free circulating estrogen.
Cause for Concern?
Why is extra circulating estrogen a concern for someone with endometriosis? Although the disease is not caused by excess estrogen, too much estrogen contributes to increased endometrial tissue growth and lesions, which is the source of all the horrible pain and problems with endometriosis! If you remember from our previous discussion on dysbiosis, most women who suffer from endometriosis also suffer from dysbiosis and IBS, which means the likelihood of them having issues with free circulating estrogen is higher. Talk about the perfect storm of unfortunate dysfunctions, to say the least.
Diagnosis for Endometriosis
Now that some light has been shed on all the complexities running simultaneously behind this frustrating disease, let’s talk about what you can do if you have it or think you may have it.
Endometriosis often develops a few years after menstruation first begins, which on average is between the ages of 10-15 years old. Commonly noted risk factors of developing endometriosis include, but are not limited to, the following: menstruation starting at an early age, never giving birth, shortened menstrual cycles, heavy and longer menstrual periods, low body mass index, family history of endometriosis, immune disorders, and disorders of the reproductive tract. Furthermore, research has found that symptoms of endometriosis can temporarily improve during pregnancy and can go away entirely once menopause occurs. 
Seek Advice from your Doctor
It is advised to see your doctor if you have any of these signs and symptoms that may indicate the presence of endometriosis. Receiving an early diagnosis for this disease can help improve outcomes with better management of symptoms, but unfortunately, the average time before diagnosis is 5-8 years! Something important to note is that during the years before an official endometriosis diagnosis, women often report receiving a diagnosis of IBS. The gut-endometriosis connection shows itself once again.
A rather invasive procedure called a laparoscopy has been coined as the gold standard for endometriosis diagnosis, but there are fortunately other less invasive options doctors can use as well. These include pelvic examinations using transvaginal ultrasound and MRI (magnetic resonance imaging) scans. Mapping a detailed history with your health professional is also critical. When it comes to the IBS symptoms within an endometriosis diagnosis, no tests currently exist to diagnose IBS, but symptoms are used for identification.
Treatments and Symptom Management
Although many women who have endometriosis also have some form of gut dysfunction, the management and approach to tackling specific symptoms between both conditions will vary.
The standard treatments currently offered for managing endometriosis symptoms include birth control pills, IUDs (intrauterine devices), and other hormone-modulating pharmaceuticals called aromatase-inhibitors and GnRH agonists. Other strategies used traditionally in western medicine are pain medication, surgical excision of endometrial lesions, and hysterectomy (surgical removal of the uterus). Unfortunately, many of these options can have potential negative side effects and none completely prevent recurrences of the endometrial lesions.
These treatments are not perfect, however, they can provide some relief to those suffering. It is clear more research, studies, and alternative approaches are needed. Above all, this is not the end of this discussion! Evidence has shown, that managing symptoms within the gut, can help manage symptoms of endometriosis, including the overlapping IBS symptoms.
Managing Symptoms through Lifestyle Changes
While more research is needed regarding the exact mechanisms and efficacies for treating the gut microbiome as a management strategy for endometriosis, steps can be made to help support overall gut health and gut symptoms, which in turn, can help manage symptoms of endometriosis. And fortunately, there are many simple lifestyle changes one can make to help improve their overall gut health! Some of these lifestyle actions for supporting a healthy gut include: eating fiber rich foods, getting adequate amounts of sleep, drinking enough water every day, maintaining an active lifestyle, and lowering stress levels on a daily basis.
Probiotics and Diet
When managing IBS symptoms, often a dietary approach is necessary. Some common foods suggested to avoid include foods with preservatives and/or artificial coloring, gluten, sugar substitutes, caffeine, chocolate, and insoluble fiber. A common diet plan that helps IBS patients is called the low FODMAP diet.
Another strategy for improving gut health is focusing on your gut microbiome balance through probiotics. Because a disturbed gut microbiome plays a large role in IBS, using probiotics is often advised to aid in the management of symptoms. The current scientific literature suggests probiotics containing either Lactobacillus and/or Bifidobacterium to help for the treatment of IBS. One study even found that using a specific strain of Lactobacillus probiotic significantly improved reported pain in endometrial patients over 12 weeks compared to a control group.
Not all Probiotics are Created Equal
Flourish probiotic contains the strains of bacteria found to help patients with gut dysbiosis and IBS. They are included in a broad ecosystem of 11 diverse living strains thriving in their most natural liquid environment. This synergistic collaboration creates a naturally acid-stable product that can actually survive the acidity of the stomach and transit to where your body needs it the most, the lower GI tract! It is important to choose a quality probiotic that can deliver the help an unbalanced gut needs and to consult with your healthcare provider. 
Concluding Statements
As you can see, endometriosis is without a doubt a challenging disease to manage. Having a better understanding of the complexities of this disease, an early diagnosis, and a well-versed and diverse medical team, can help result in better management of symptoms, which every human being deserves!
Certainly, more studies and supportive treatments for endometriosis are needed, as well as continued research exploring the gut’s connection to this disease. It is the hope, that through understanding the underlying mechanisms behind endometriosis more clearly, progress can be made for better treatment options and alleviation of all the suffering that can accompany endometriosis. To those possibly going through an endometriosis battle, please know you are not alone nor forgotten. 
The content in this post is not intended to be professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition.
Written by Kelsy Armstrong, Entegro Health
Sources:
- Ahn S.H., Monsanto S.P., Miller C., et al. “Pathophysiology and Immune Dysfunction in Endometriosis.” Biomed Res Int. 2015;2015:795976.
- Arvonen M., Berntson L., Pokka T., Karttunen T.J., Vähäsalo P., Stoll M.L. “Gut Microbiota-host Interactions and Juvenile Idiopathic Arthritis.” Pediatr Rheumatol Online J. 2016;14:44.
- Ata B., Yildiz S., Turkgeldi E., Brocal V.P., Dinleyici E.C., Moya A., Urman B. “The Endobiota Study: Comparison of Vaginal, Cervical and Gut Microbiota Between Women with Stage 3/4 Endometriosis and Healthy Controls.” Sci Rep. 2019;9: 2204. doi:10.1038/s41598-019-39700
- Baker J.M., Al-Nakkash L., Herbst-Kralovetz M.M. “Estrogen-gut Microbiome Axis: Physiological and Clinical Implications.” Maturitas. 2017;103:45–53.
- Clinning K., N.D. “The Relationship Between Gut Health and Endometriosis.” Women’s Health, Aug. 2019, https://www.whitelotusclinic.ca/gut-health-and-endometriosis.
- Dalal, A. “Endometriosis and Gut Health Are Linked. An Expert Tells You All About How the Condition Affects the Gut and Bowel Function.” Sept. 2021, https://www.healthshots.com/intimate-health/menstruation/how-are-endometriosis-and-gut-health-related-and-what-are-the-symptoms/.
- Dieterich W, Schink M, and Zopf Y. “Microbiota in the Gastrointestinal Tract.” Med Sci. 2018;6(4).
- DiVasta A.D., Vitonis A.F., Laufer M.R., Missmer S.A. “Spectrum of Symptoms in Women Diagnosed with Endometriosis During Adolescence vs Adulthood.” Am J Obstet Gynecol. 2018;218:324e1–324e11.
- Giudice L.C., Kao L.C. “Endometriosis.” Lancet. 2004;364:1789–99.
- Jess T., Frisch M., Jørgensen K.T., Pedersen B.V., Nielsen N.M. “Increased Risk of Inflammatory Bowel Disease in Women with Endometriosis: A Nationwide Danish Cohort Study.” Gut. 2012;61: 1279–1283. doi:10.1136/gutjnl-2011-301095.
- Karmarkar D., Rock K.L. “Microbiota Signaling Through MyD88 is Necessary for a Systemic Neutrophilic Inflammatory Response.” Immunology. 2013;140:483–92.
- Laschke M.W., Menger M.D. “The Gut Microbiota: A Puppet Master in the Pathogenesis of Endometriosis?” Am J Obstet Gynecol. 2016;215(1):68–e1-4.
- Leonardi M., Hicks C., El-Asseed F., et al. “Endometriosis and the Microbiome: A Systematic Review.” Bjog. 2020;127:239–49.
- “Endometriosis Care at Mayo Clinic.” July 2018, https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc- 20354656.
- Rizk B., Fischer A.S., Lofty H.A., Turki R., Zahed H.A., Malik R., Holliday C.P., Glass A., Fishel H., Soliman M.Y., et al. “Recurrence of Endometriosis After Hysterectomy.” Facts Views Vis Obgyn. 2014;6: 219-227.
- Saidi K., Sharma S., Ohlsson B. “A Systematic Review and Meta-analysis of the Associations Between Endometriosis and Irritable Bowel Syndrome.” Eur J Obstet Gynecol Reprod Biol. Mar. 2020;246:99-105. doi: 10.1016/j.ejogrb.2020.01.031. Epub 2020 Jan 25. PMID: 32004880.
- Chadchan B.C., Popli P., Ambati C.R., Tycksen E., Han S.J., Bulun S.E., Putluri N., Biest S.W., Kommagani R. “Role for Short-chain Fatty Acids in Endometriosis.” Kommagani Life Science Alliance. Sept. 2021;4 (12) e202101224; DOI: 10.26508/lsa.202101224.
- Svensson A., Brunkwall L., Roth B., et al. “Associations Between Endometriosis and Gut Microbiota.” Reprod. Sci. 2021;28, 2367–2377. https://doi.org/10.1007/s43032-021-00506-5.
- Vercellini P., Vigano P., Somigliana E., et al. “Endometriosis: Pathogenesis and Treatment.” Nat Rev Endocrinol. 2014;10:261–75.
- Wolski C. “Endometriosis and Gut Health.” Sept. 2020, https://healthyeatingclinic.com.au/endometriosis-and-gut-health/.
- Zhang Q., Shen Q., Celestino J., et al. “Enhanced Estrogen-induced Proliferation in Obese Rat Endometrium.” Am J Obstet Gynecol. 2009;200:186–e1-8.
- Zhang X., Xu H., Lin J., Qian Y., Deng L. “Peritoneal Fluid Concentrations of Interleukin-17 Correlate with the Severity of Endometriosis and Infertility of This Disorder.” Bjog. 2005;112:1153–5.

 New customers! Get 11% OFF your first Flourish order with Code FRESHSTART11
New customers! Get 11% OFF your first Flourish order with Code FRESHSTART11